Tips for a Successful Patient Safety Huddle
Commitment to Continuous Quality Improvement requires regular communication on quality and safety issues. An important way of helping achieve this is through dedicated ‘Patient Safety Huddles’ or ‘Patient Safety Review Meetings’.
A huddle is a short stand-up meeting and can be an effective method of communicating important safety issues in time-poor environments such as healthcare organisations. It is often held before the start of the workday. The frequency, format and length of the huddle will vary based on practice setting, level of risk associated with the services offered and team size. The huddle provides a way for your team to maintain focus on patient safety in an open environment, allowing for review and implementation of relevant Quality Improvement Initiatives. The huddle aids in identifying potential safety issues proactively instead of reactively.
The following are some helpful tips for a successful ‘Patient Safety Huddle’ in your organisation:
Tips for a Successful Patient Safety Huddle
- Have a set time and place: Choose a consistent time, frequency and location (e.g. once a month in the dispensary). Based on team size and shift patterns, it may be worthwhile having a meeting in the morning and at the end of the day to capture the voice of the full team. Be agile– meetings may also need to be scheduled ad hoc (e.g. following a serious safety incident or practice change).
- Involve the whole team and assign roles: Promote team engagement and actively seek their input before, during and after the meeting. It can be useful to ask each team member to bring one patient safety topic and suggested solution to each meeting to encourage involvement. The team will be invested in improvement if they are involved in decision-making and the development and improvement of processes, and are given the opportunity to develop and use their skills for Quality Improvement. Roles should be assigned to ensure there is clear accountability. One person (e.g. Patient Safety Lead) should lead the meeting and ensure associated actions are documented and assigned. Buy-in is also required at all levels of the organisation, including senior management, who will need to understand the value of investing time and resources to carry out the meetings and complete associated actions.
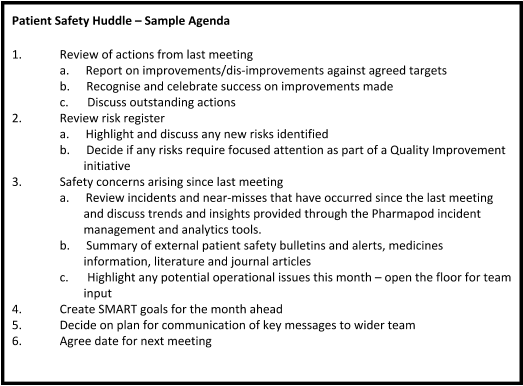
- Create and communicate an agenda: The Patient Safety Lead should seek input from relevant stakeholders and team members. They will also need to review the agreed actions from the previous huddle and provide an update at the meeting. Data should be collated from internal (e.g. incident and near miss data from Pharmapod) and external sources (e.g. patient safety bulletins and alerts, medicines information, literature and journal articles). A sample agenda is provided below.
- Think about tone and language: Patient Safety Huddles are an important step towards creating a Patient Safety Culture within your organisation – open dialogue should be encouraged and the team should feel listened to without fear of judgement or punitive action. If you are leading the huddle, think about tone and language used during the meeting to try to make it a positive experience for everyone involved.
- Provide a visual display: Support your meeting with a physical display in the pharmacy to post huddle information, agendas, Pharmapod incident data as well as information on patient safety relevant to your practice setting. Using outputs from data from the Pharmapod platform during the meeting in real-time will help the team see the benefits of recording incidents.
- Be ready to act – document and assign actions: The huddles will often trigger Quality Improvement Initiatives. These may be quick wins or longer-term goals. For example, based on the identified areas for improvement, relevant SOPs may be optimised based on feedback or best practice guidance. Through the use of the Pharmapod platform, actions can be assigned to team members to ensure next steps are completed. When creating and assigning actions, you should ensure they are SMART (i.e. Smart, Measurable, Attainable, Realistic and Time-bound).
- Document and Communicate Actions: If it isn’t documented, it didn’t happen! By documenting the agenda and outputs from each meeting, reviewing updated Pharmapod data, and gauging the team’s understanding and completion of actions, each pharmacy can evaluate their progress and demonstrate their commitment to Continuous Quality Improvement.
- Build it into your process: The process for patient safety huddles or review meetings should be built into your organisation’s SOPs (or it may need a dedicated SOP of its own). This will ensure that everyone, including new team members, understand the purpose and process. Templates are useful to ensure information and actions are recorded consistently at each meeting. The Patient Safety Review within Pharmapod is ideal for this.